Dexamethasone: A Comprehensive Overview from an Anesthesia Perspective
Dexamethasone is a potent, long-acting glucocorticoid that has become an indispensable tool in the modern anesthesiologist's perioperative armamentarium. Far from its use in chronic inflammatory diseases, its utility in the operating room centers on three core principles: potent anti-emesis, reduction of tissue edema, and opioid-sparing analgesia. Its inclusion in multimodal regimens is a cornerstone of Enhanced Recovery After Surgery (ERAS) protocols.
Mechanism of Action (MoA)
The perioperative benefits of dexamethasone are derived from its powerful glucocorticoid (anti-inflammatory) activity, with minimal mineralocorticoid (salt-retaining) effects.
- Anti-inflammatory Action: Dexamethasone penetrates cell membranes and binds to cytoplasmic glucocorticoid receptors. This complex moves into the nucleus to inhibit the transcription of inflammatory mediators, most notably by blocking phospholipase A2. This prevents the formation of prostaglandins and leukotrienes, which are key drivers of inflammation, pain, and edema.
- Antiemetic Action: The exact mechanism is multifactorial and not fully understood. It is believed to work centrally by:
- Reducing prostaglandin synthesis in the chemoreceptor trigger zone (CTZ) of the brainstem.
- Potentially releasing endorphins that provide an anti-emetic effect.
- Inhibiting serotonin release from enterochromaffin cells in the gut.
- Metabolic Effects: It promotes gluconeogenesis, which can lead to hyperglycemia, a critical consideration in the perioperative period, especially for diabetic patients.
Therapeutic Uses (Indications)
The anesthesiologist uses dexamethasone for targeted, short-term perioperative goals.
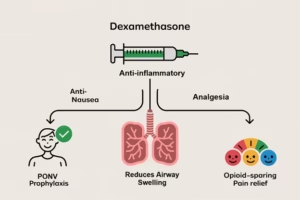
- Prophylaxis of Post-Operative Nausea and Vomiting (PONV): This is its most common indication. It is a first-line agent for PONV prophylaxis, particularly in high-risk patients or for surgeries with a high incidence of PONV (e.g., laparoscopic, gynecologic, strabismus surgery).
- Reduction of Airway and Tissue Edema: It is routinely administered for procedures where swelling can compromise the airway or cause significant pain.
- ENT Surgery: Tonsillectomy, adenoidectomy, airway reconstruction.
- Neurosurgery & Spine Surgery: To reduce cerebral or spinal cord edema.
- Thyroid and Maxillofacial Surgery: To reduce airway swelling and improve patient comfort.
- Opioid-Sparing Analgesia: As part of a multimodal analgesia plan, its anti-inflammatory properties reduce postoperative pain, particularly for orthopedic and dental procedures, thereby decreasing the need for opioids.
- Adjunct in Regional Anesthesia: When added to local anesthetics for intrathecal or epidural anesthesia, it can prolong the duration of both sensory and motor blockade.
- Adjunct in Anaphylaxis: Used as a secondary agent after epinephrine to prevent biphasic or prolonged allergic reactions.
Administration and Dosage
- Route: Most commonly administered intravenously (IV). Can also be given orally, intramuscularly (IM), or intrathecally/epidurally (preservative-free formulation required).
- Dosing: Dose is indication-dependent.
- PONV Prophylaxis: 4 to 8 mg IV is the standard dose, given at induction of anesthesia.
- Anti-edema / Analgesia: A higher dose of 0.1 to 0.2 mg/kg IV (typically 8-10 mg for an adult) is more effective.
- Intrathecal/epidural: 0.1 to 0.2 mg of preservative-free dexamethasone.
- Timing: For optimal effect, it should be administered before the surgical incision (pre-emptively) to allow time for the genomic effects to manifest.
Pharmacokinetics
- Onset of Action: The anti-emetic effect begins within 1-2 hours, while the peak anti-inflammatory effect can take several hours.
- Half-life: This is a key feature. It has a plasma half-life of ~3-4 hours but a biological half-life of 36-72 hours. This prolonged duration explains its sustained anti-inflammatory and anti-emetic effects from a single dose.
- Metabolism: Metabolized primarily in the liver.
- Excretion: Metabolites are excreted by the kidneys.
Adverse Effects and Side Effects
With single-dose perioperative use, side effects are generally mild but clinically important.
- Perineal Irritation: A common, transient burning or stinging sensation in the perineal area upon IV injection. This can be mitigated by diluting the drug and injecting it slowly.
- Hyperglycemia: The most significant metabolic side effect. Blood glucose can rise for 24-48 hours post-administration.
- Mood Changes: Can cause euphoria, agitation, or, rarely, confusion.
- Delayed Wound Healing / Increased Infection Risk: A theoretical concern, primarily associated with high or repeated doses.
Contraindications and Cautions
-
Contraindications:
- Known hypersensitivity to dexamethasone.
- Systemic fungal infection (unless specific anti-fungal therapy is instituted).
-
Cautions:
- Diabetes Mellitus: This is the most important caution. Requires careful perioperative blood glucose monitoring and management.
- Active Peptic Ulcer Disease: Can increase the risk of gastrointestinal bleeding.
- Psychiatric Disorders: Can exacerbate psychosis or severe mood disorders.
- Active Infection: May mask signs of infection like fever.
Monitoring Parameters
Monitoring is focused on the desired effects and potential adverse outcomes.
- Blood Glucose: Check pre-operatively and at regular intervals post-operatively in all patients, especially diabetics.
- Incidence of PONV: The primary therapeutic outcome to assess.
- Pain Scores: To evaluate the opioid-sparing analgesic effect.
- Airway Patency: For cases where it was used for anti-edema (e.g., post-tonsillectomy).
- Mental Status: Monitor for agitation or confusion in the post-anesthesia care unit (PACU).
Key Considerations and Clinical Pearls
- Give it Early: Its delayed onset means it is most effective when given at or before induction of anesthesia, not at the end of the case.
- Dose for the Indication: 4 mg is great for PONV, but 8-10 mg is superior for analgesia and anti-edema. Choose your dose based on your primary goal.
- The Diabetic Patient is a High Priority: Always check a finger-stick glucose before giving dexamethasone and have a plan for managing postoperative hyperglycemia. The benefits often outweigh the risks, but vigilance is key.
- It's a Multimodal Team Player: Dexamethasone is not a standalone solution. Its power is realized when combined with other antiemetics (e.g., ondansetron) and analgesics (e.g., NSAIDs, acetaminophen) as part of a balanced, multimodal strategy.
- Don't Expect Immediate PONV Relief: Its effect is delayed. For treating established PONV in the PACU, a faster-acting agent like ondansetron is preferred. Dexamethasone is for prevention.
Conclusion
From an anesthesia perspective, dexamethasone is a versatile and highly effective pharmacologic agent. Its roles in preventing PONV, reducing edema, and providing opioid-sparing analgesia make it a fundamental component of modern, patient-centered perioperative care. While its side effect profile is generally favorable for single-dose use, the potential for significant hyperglycemia demands respect and proactive management. When used judiciously, it significantly improves patient comfort and outcomes.


