An In-Depth Guide to Automated Anesthesia Delivery Systems ("Anesthesia Robots")
1. What Are They?
Automated Anesthesia Delivery Systems (AADS) are sophisticated, computer-controlled platforms designed to automatically administer and adjust anesthetic drugs based on real-time patient physiological data. The term "Anesthesia Robot" is a popular but somewhat misleading moniker; these are not humanoid machines standing over the patient, but rather integrated systems of monitors, software, and infusion pumps working in a closed-loop configuration.
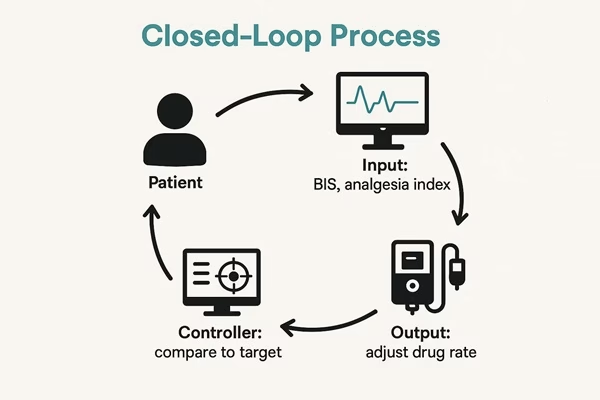
The core principle is closed-loop control, a concept borrowed from engineering. In a closed-loop system:
- A variable is continuously measured (e.g., the patient's depth of hypnosis).
- This measurement is compared to a pre-set target value.
- The system automatically adjusts an output (e.g., the infusion rate of a hypnotic drug) to minimize the difference between the measured value and the target.
Think of it like a thermostat: it measures room temperature (input), compares it to your desired temperature (target), and turns the furnace on or off (output) to maintain it. An AADS does the same for anesthesia.
2. What is the Need for Them? (The Rationale)
Modern anesthesia is a delicate balancing act. The anesthesiologist must simultaneously manage the patient's level of unconsciousness (hypnosis), pain relief (analgesia), and muscle relaxation (paralysis), all while maintaining stable vital signs (blood pressure, heart rate, etc.). This complex task is prone to several challenges that automation aims to address:
- Human Error and Cognitive Load: Anesthesiologists manage dozens of variables at once, especially during long or complex surgeries. Fatigue or distraction can lead to errors in judgment or drug titration.
- Inter-patient Variability: Patients react to anesthetic drugs in vastly different ways based on age, weight, genetics, and co-morbidities. A dose that is perfect for one patient may be too much or too little for another.
- Standardization of Care: Manual anesthesia delivery can vary significantly between providers. Automation offers the potential to deliver a more consistent, evidence-based standard of care, reducing variability and potentially improving outcomes.
- Efficiency: By automating the routine, minute-to-minute task of drug titration, an AADS can free the anesthesiologist to focus on higher-level clinical decision-making, such as anticipating surgical events, managing complex fluid shifts, and responding to emergencies.
- Drug Optimization: Automated systems can deliver drugs with a precision that is difficult to achieve manually, potentially reducing overall drug consumption, minimizing side effects (like postoperative nausea and vomiting), and lowering costs.
3. How Do They Work? (The Technology)
An AADS is composed of three main components, each corresponding to a part of the closed-loop.
A. The Input (Sensing/Measurement):
This is how the system "knows" what's happening to the patient. It relies on advanced, specialized monitors to quantify aspects of anesthesia that were once subjective.
- Depth of Hypnosis (Unconsciousness): The most mature and widely used input is the Bispectral Index (BIS) or similar EEG-based monitors. A sensor on the patient's forehead measures brainwave activity and converts it into a single number (0-100). A BIS of 40-60 is generally considered an appropriate target for general anesthesia.
- Analgesia (Pain/Nociception): This is the most challenging variable to measure. The system cannot "ask" the patient if they are in pain. Instead, it uses surrogates like the Analgesia Nociception Index (ANI), which analyzes changes in heart rate variability caused by painful stimuli (like surgical incision). A high ANI suggests good analgesia, while a dropping ANI suggests the patient is experiencing nociception and needs more opioid.
- Muscle Relaxation (Paralysis): Measured using Train-of-Four (TOF) monitoring, where a nerve is stimulated and the muscle response is measured. The system can adjust the infusion of muscle relaxants to maintain a specific number of twitches.
- Hemodynamics: Standard monitors provide blood pressure and heart rate data, which can be integrated into the system's decision-making algorithm.
B. The Controller (The "Brain"):
This is the software algorithm, the heart of the AADS. It takes the input data (e.g., BIS = 55) and compares it to the target set by the anesthesiologist (e.g., BIS target = 50). Based on the difference, it calculates the precise change needed in the drug infusion rate. These algorithms often use PID (Proportional-Integral-Derivative) controllers, a standard control theory method that provides smooth and responsive adjustments.
C. The Output (Actuation):
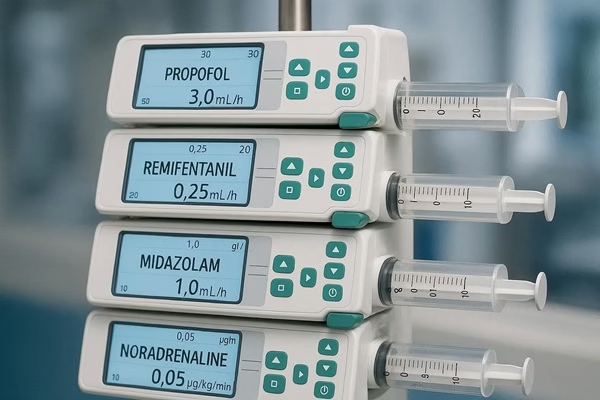 The controller's command is sent to one or more syringe infusion pumps. Each pump is dedicated to a specific drug (e.g., a hypnotic like propofol, an opioid like remifentanil, and a muscle relaxant). The AADS can increase, decrease, or stop the infusion of each drug independently to achieve its goals.
The controller's command is sent to one or more syringe infusion pumps. Each pump is dedicated to a specific drug (e.g., a hypnotic like propofol, an opioid like remifentanil, and a muscle relaxant). The AADS can increase, decrease, or stop the infusion of each drug independently to achieve its goals.
4. Benefits and Potential Advantages
- Enhanced Patient Safety: By maintaining a more stable depth of anesthesia, AADS can significantly reduce the risk of intraoperative awareness. They also prevent the large swings in drug concentration that can cause hemodynamic instability.
- Increased Drug Precision: The system delivers exactly what is needed, when it is needed, reducing total drug usage and associated side effects like PONV and delayed recovery.
- Improved Consistency: Every patient is managed according to the same, evidence-based protocol, reducing provider-dependent variability.
- Data for Research: These systems generate massive, high-resolution datasets on drug administration and patient response, which are invaluable for improving anesthetic practices and developing smarter algorithms.
- Empowering the Anesthesiologist: By handling the routine, the system allows the human anesthesiologist to be a true perioperative physician, focusing on the entire patient and the surgical course.
5. Challenges, Limitations, and Concerns
Despite the promise, significant hurdles remain before AADS become standard of care.
- The "Black Box" Problem: The anesthesiologist may not always understand the complex reasoning behind the algorithm's decision, which can be unsettling when a patient's condition is critical.
- Sensor Failure and Artifacts: What happens if a BIS sensor falls off or gets covered by surgical drapes? The system might misinterpret the resulting "flatline" signal as a very deep anesthetic state and stop all drugs, risking awareness, or it might not react at all. Robust fault detection and alarm systems are absolutely critical.
- Lack of Context: An algorithm has no understanding of the surgical context. It doesn't know that the surgeon is about to make a painful incision or that there has been a sudden, massive hemorrhage. It can only react to the physiological data after the event has occurred.
- The Analgesia Challenge: As mentioned, reliably measuring pain in an unconscious patient remains the weakest link. Without a perfect analgesia monitor, the loop can never be fully closed.
- Legal and Ethical Liability: Who is responsible if the automated system makes a mistake? The supervising anesthesiologist? The hospital? The device manufacturer? This legal gray area is a major barrier to widespread adoption.
- Cost and Integration: These systems are expensive and require seamless integration with a wide array of existing hospital equipment, which is a significant technical and logistical challenge.
6. Current Status and Future Outlook
Currently, no fully integrated, multi-loop AADS is approved for widespread use in the United States. However, single-loop systems (e.g., a closed-loop for propofol based on BIS) have been developed and used in research and clinical settings in Europe and Asia (e.g., the "McSleepy" system).
The future of AADS is likely tied to advancements in Artificial Intelligence (AI) and Machine Learning:
- Predictive Analytics: Future AI-driven systems could analyze patient data to predict hemodynamic events (like hypotension) before they happen, allowing for pre-emptive intervention.
- Personalized Medicine: Algorithms could be trained on vast datasets to create a unique anesthetic "profile" for each patient before the case even begins, based on their pre-operative data.
- Full Integration: The ultimate goal is a multi-loop system that seamlessly manages hypnosis, analgesia, hemodynamics, and fluid therapy simultaneously.
7. The Role of the Anesthesiologist: The Human in the Loop
It is crucial to understand that the goal of AADS is not to replace the anesthesiologist. Rather, it is to augment their capabilities and change their role.
The anesthesiologist will transition from being a "manual pilot" to a highly skilled supervisor, strategist, and safety net. They will set the goals, monitor the system's performance, manage the complex context that the algorithm cannot understand, and intervene instantly for unexpected events or emergencies. The human judgment, experience, and crisis management skills of the anesthesiologist remain the most important safety feature in the operating room. The "robot" is simply a powerful tool to help them do their job even better.