The Endotracheal Tube - A Foundation of Modern Medicine
 An endotracheal tube is a flexible catheter that is inserted directly into the trachea (windpipe) through the mouth or nose. This procedure, known as endotracheal intubation, creates a secure, patent airway directly to the lungs.
An endotracheal tube is a flexible catheter that is inserted directly into the trachea (windpipe) through the mouth or nose. This procedure, known as endotracheal intubation, creates a secure, patent airway directly to the lungs.
Part 1: Primary Purposes of Intubation
- Airway Protection: The most critical function. By sealing the trachea with an inflatable cuff, the ETT prevents the aspiration of gastric contents, blood, or other foreign materials into the lungs.
- Ventilation: It provides a direct conduit for a mechanical ventilator to deliver positive-pressure breaths to a patient who is unable to breathe adequately on their own.
- Oxygenation: It allows for the delivery of high concentrations of oxygen.
- Airway Access: It provides a route for administering certain drugs (e.g., epinephrine, atropine) directly into the tracheobronchial tree during cardiac arrest (though this is now a secondary route).
- Facilitation of Pulmonary Hygiene: It allows for suctioning of secretions from the lower airway.
Anatomy of a Standard Endotracheal Tube
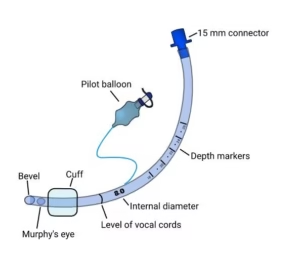
While variations exist, a standard cuffed ETT has several key components:
- Connector/15mm Adapter: The standard fitting at the proximal end that connects to the breathing circuit, ambu-bag, or ventilator.
- Pilot Balloon: A small, external balloon that inflates and deflates along with the main cuff, providing a visual indicator of cuff inflation status.
- Inflation Line & Valve: A thin tube connecting the pilot balloon to the main cuff. The valve allows air to be introduced into the system and prevents it from escaping.
- Shaft: The main body of the tube, typically made of medical-grade polyvinyl chloride (PVC). It has distance markings (in centimeters) to gauge the depth of insertion.
- Cuff: An inflatable balloon near the distal tip that, when inflated, seals the trachea. Modern cuffs are "high-volume, low-pressure" to minimize the risk of tracheal wall ischemia.
- Bevel: The angled slant at the tip of the tube, designed to facilitate passage through the vocal cords with minimal trauma.
- Murphy's Eye: A small hole on the side of the tube, just above the bevel. It serves as a safety vent, allowing for ventilation if the main opening of the tube becomes occluded (e.g., by abutting the tracheal wall).
Part 2: A History of the Endotracheal Tube
The journey to the modern ETT is a story of innovation driven by the need to control the airway.
Ancient and Early Attempts: The concept of a surgical airway dates back thousands of years, with tracheostomy described in ancient Egyptian and Indian texts. However, these were crude procedures with high mortality rates. The idea of a non-surgical airway was centuries away.
The 19th Century - The First True Intubations:
- 1844: Horace Green, a New York physician, is credited with performing the first successful orotracheal intubation on a patient using a silver tube to treat diphtheria.
- 1869: German surgeon Friedrich Trendelenburg pioneered the surgical technique of tracheal intubation for anesthesia during head and neck surgery.
- Late 1800s: Sir William Macewen in Scotland developed a systematic technique for blind orotracheal intubation using a metal tube, primarily for patients with airway obstruction from tumors or diphtheria. He is often called the "Father of Modern Intubation."
The Early 20th Century - The Age of Visualization:
- 1913: Chevalier Jackson, an American laryngologist, designed a laryngoscope and a straight metal tube, standardizing the technique for direct laryngoscopy. His work transformed intubation from a blind art into a visualized procedure.
- 1943: Sir Robert Macintosh, a New Zealand anesthesiologist, introduced the curved laryngoscope blade that bears his name. This design, which lifts the epiglottis indirectly, became the most widely used blade in the world and remains a standard today.
The Mid-20th Century - The Cuff Revolution:
- Pre-1950s: ETTs were uncuffed. Positive pressure ventilation was risky as it could easily leak air, leading to inadequate ventilation and a high risk of aspiration.
- 1950s: The invention of the inflatable cuff was a monumental leap. Early cuffs were "low-volume, high-pressure," which could seal the airway but often cut off blood flow to the tracheal mucosa, leading to necrosis and stenosis.
- Late 1960s-1970s: The development of the high-volume, low-pressure (HVLP) cuff solved this problem. These cuffs distribute pressure over a larger area of the trachea, creating an effective seal while significantly reducing the risk of ischemic injury. This made long-term mechanical ventilation feasible and safe.
Late 20th Century to Present - Specialization and Safety:
- Materials: Shift from red rubber to clear PVC, which is softer, less reactive, and allows for visualization of secretions.
- Specialized Tubes: The latter half of the century saw an explosion of specialized designs: double-lumen tubes for thoracic surgery, armored tubes to prevent kinking, laser-resistant tubes for airway surgery, and tubes with subglottic suction ports to prevent pneumonia.
- Modern Innovations: The focus has shifted to enhancing safety and usability with features like electromagnetic tracking for difficult intubations and improved cuff materials to minimize micro-aspiration.
Part 3: Types of Endotracheal Tubes and Their Specific Uses
The "one-size-fits-all" approach is obsolete. Modern medicine requires a variety of ETTs tailored to specific patient needs and surgical procedures.
a) Standard Cuffed vs. Uncuffed Tubes
- Cuffed Tubes (HVLP): The standard for adults and increasingly for children. Used for any case requiring positive pressure ventilation or a high risk of aspiration.
- Uncuffed Tubes: Traditionally used in children under 8 years old because their narrow cricoid cartilage naturally forms a seal. However, cuffed pediatric tubes with specially designed low-pressure cuffs are now more common as they provide a better seal and reduce the need for tube exchanges, without increasing the risk of injury when sized correctly.
b) Tubes Based on Material and Construction
- Standard PVC Tube: The most common type. Inexpensive, clear, and has good memory. It can become stiff at low temperatures, so it is often warmed before use.
- Armored/Reinforced Tube: Has a metal or nylon braid embedded within the PVC wall.
- Use: Neurosurgery, head and neck surgery, or any procedure where the patient's head and neck will be positioned in extreme angles. The reinforcement prevents the tube from kinking and occluding the airway.
- Silicone Tube: Softer and more biocompatible than PVC.
- Use: Patients requiring long-term intubation (e.g., tracheal stenosis) or those with severe latex/PVC allergies.
c) Tubes Based on Specialized Function
Double-Lumen Endobronchial Tube (DLT): Essentially two tubes in one—a long tracheal lumen and a shorter bronchial lumen that is advanced into one of the mainstem bronchi (usually the left). Each lumen has its own cuff and pilot balloon.
- Use: Thoracic surgery. It allows for one-lung ventilation (OLV), where one lung is isolated and deflated to give the surgeon a clear field to operate on the chest (e.g., for lung resection, esophageal surgery, or repairing an aortic aneurysm).
Bronchial Blocker: A balloon-tipped catheter that is inserted through a standard ETT. The balloon is advanced into a mainstem bronchus under bronchoscopic guidance and inflated to block that lung.
- Use: An alternative to a DLT for one-lung ventilation. It is particularly useful if a patient is already difficult to intubate with a large DLT, or if a patient is already intubated with a standard tube and later requires lung isolation.
Pre-formed Tubes: Shaped to specific angles to keep the tubing away from the surgical field.
- RAE (Ring, Adair, and Elwyn) Tubes: Come in both nasal (NRAE) and oral (ORAE) versions. The tube is pre-curved to run over the forehead or chin, respectively.
- Use: Oral, maxillofacial, or head and neck surgery where the breathing circuit must be completely out of the surgeon's way.
Laser-Resistant Tube: Specifically designed to prevent ignition from surgical lasers used on the airway.
- Construction: The PVC is impregnated with a reflective material (like aluminum or silver) and may have a second external cuff.
- Use: Laryngeal or tracheal laser surgery (e.g., for papillomas or carcinoma). Using a standard PVC tube in this setting is extremely dangerous as it can ignite, causing a catastrophic airway fire.
Microlaryngeal Tube (MLT): A very small-diameter, specially designed tube.
- Use: Microsurgery of the larynx. Its small outer diameter provides the surgeon with maximal visualization of the vocal cords, while its short length reduces resistance. The trade-off is higher airway resistance and more difficult ventilation/suctioning for the anesthesiologist.
Endotracheal Tube with Subglottic Suction Port: A standard ETT with an additional port and lumen that opens just above the cuff.
- Use: Intensive Care Units (ICU). A dedicated suction line can be connected to this port to continuously or intermittently remove secretions that pool in the subglottic space above the cuff. This has been shown to significantly reduce the incidence of Ventilator-Associated Pneumonia (VAP).
Electromagnetic (EM) Stylet-Compatible Tubes: These tubes are designed to be used with an electromagnetic navigation system (e.g., the Airway Scope or other EM tracking devices). A stylet with an electromagnetic sensor is placed inside the tube.
- Use: Difficult or anticipated difficult airways. The system provides a real-time, 3D view of the tube tip's position relative to the patient's airway on a monitor, guiding the practitioner toward the glottis, even when the view is poor.
Conclusion
The endotracheal tube has evolved from a simple metal cannula to a sophisticated, highly specialized medical device. Its development has paralleled and enabled the advancement of surgery, critical care, and emergency medicine. Understanding the history and, more importantly, the specific design and purpose of each type of ETT is fundamental knowledge for any clinician responsible for managing a patient's airway. The choice of tube is not a trivial one; it is a critical decision that directly impacts patient safety, surgical success, and clinical outcomes.
Next: Endotracheal Tube Sizing and Selection →Page 1 of 2
Part 4: Endotracheal Tube Sizing and Selection
Choosing the correct endotracheal tube (ETT) is a critical decision. The primary measurement is the Internal Diameter (ID) in millimeters (mm), which determines the resistance to airflow and the ease of suctioning. The Outer Diameter (OD) is also crucial, as it must fit through the vocal cords or nostril without causing trauma.
A tube that is too small increases airway resistance, makes ventilation difficult, and hampers effective suctioning. A tube that is too large can cause severe trauma to the larynx and trachea, leading to post-extubation stridor, scarring, and stenosis.
Sizing for Adult Patients
In adults, sizing is less formulaic and more based on patient demographics and clinical context.
Patient Group | Internal Diameter (ID) | Key Considerations |
|---|---|---|
| Average Adult Female | 7.0 mm - 7.5 mm | A 7.0 mm tube is standard. A 6.5 mm may be used for a very small woman or for nasal intubation. |
| Average Adult Male | 8.0 mm - 8.5 mm | An 8.0 mm tube is standard. An 8.5 mm tube is used for larger men or when a large suction catheter or bronchoscope might be needed. |
| Nasal Intubation | 6.5 mm - 7.5 mm | A smaller size (typically 0.5-1.0 mm smaller than for oral intubation) is required to pass safely through the nasal passage. |
| Thoracic/Lung Surgery | 8.0 mm - 9.0 mm (Left) | A larger tube is preferred to accommodate a large suction catheter or a flexible bronchoscope, which is often used to confirm the position of a double-lumen tube. |
| Anticipated Difficult Airway | 6.0 mm - 7.0 mm | A smaller tube may be easier to insert through a restricted glottic opening. A tube exchanger can then be used to swap it for a larger tube if needed after the airway is secured. |
Sizing for Pediatric Patients
In children, sizing is more precise and calculated using formulas based on age, as the airway anatomy changes rapidly with growth. The narrowest part of a child's airway is the cricoid cartilage, which is circular. This is why uncuffed tubes were traditionally used, as the cricoid itself provided the seal.
Formulas for Uncuffed Tubes (Historically Standard):
- Size (Internal Diameter in mm):
(Age in years + 16) / 4 - Insertion Depth (cm at the lips):
(Age in years / 2) + 12
The Shift to Cuffed Tubes in Pediatrics: Modern, low-pressure cuffed tubes (especially those with a tapered profile like the Microcuff®) are now standard for most children over 1 year old, and even infants in many institutions. The benefits are a more reliable seal, reduced leak, and lower incidence of post-extubation stridor. When using a cuffed tube, you can often use the same formula but may choose a size 0.5 mm smaller to ensure the cuff doesn't need to be over-inflated to achieve a seal.
Formulas for Cuffed Tubes (Modern Practice):
- Size (Internal Diameter in mm):
(Age in years + 16) / 4(or(Age / 4) + 3.5in some guidelines) - Insertion Depth (cm at the lips):
(Age in years / 2) + 12(or3 x tube IDas a simpler rule)
Sizing for Neonates and Infants
For neonates and infants less than one year old, sizing is based on weight or gestational age, not the age-based formula.
Patient Weight | Gestational Age | Uncuffed ETT Size (ID mm) | Cuffed ETT Size (ID mm) | Insertion Depth (cm at lips) |
|---|---|---|---|---|
| < 1 kg | < 28 weeks | 2.5 | 2.5 (uncuffed) | 6 - 7 |
| 1 - 2 kg | 28 - 34 weeks | 3.0 | 3.0 | 7 - 8 |
| 2 - 3 kg | 34 - 38 weeks | 3.5 | 3.0 - 3.5 | 8 - 9 |
| 3 - 5 kg | Term - 6 months | 4.0 | 3.5 | 9 - 10 |
| 5 - 7 kg | 6 - 12 months | 4.5 | 4.0 | 10 - 11 |
Part 5: Endotracheal Tube Cuff Types
The cuff is the component responsible for sealing the trachea. Its design has evolved significantly to maximize sealing efficiency while minimizing harm to the tracheal wall.
1. High-Volume, Low-Pressure (HVLP) Cuffs
This is the modern standard for almost all adult and pediatric cuffed ETTs.
- Design: A large balloon made of polyvinyl chloride (PVC) that, when inflated, achieves a large surface area of contact with the trachea.
- Mechanism: Because the pressure is distributed over a large area (following the law of physics, Pressure = Force / Area), it can create an effective seal at a low pressure (ideally < 25-30 cm H₂O).
- Advantage: Drastically reduces the risk of tracheal wall ischemia (cutting off blood flow) compared to older cuff types.
- Disadvantage: When inflated, the large PVC balloon forms inevitable folds. These channels can allow secretions from the oropharynx to leak past the cuff, leading to micro-aspiration, which is a primary cause of Ventilator-Associated Pneumonia (VAP).
2. Low-Volume, High-Pressure (LVHP) Cuffs
- Design: A small, stiff balloon that requires high pressure to expand and seal the trachea.
- Status: Largely obsolete. These cuffs were notorious for causing tracheal necrosis, scarring, and stenosis due to the high focal pressure they exerted on the tracheal mucosa. You will not encounter these in modern practice except in very specific, rare niche applications.
3. Tapered / Shaped Cuffs
This is a modern innovation designed to overcome the folding problem of standard HVLP cuffs.
- Design: The cuff is shaped like a cone or a barrel, tapering towards the distal tip. It is made from a thinner, more compliant material like polyurethane.
- Mechanism: The tapered shape allows it to conform more precisely to the shape of the trachea, significantly reducing or eliminating the folds that cause micro-aspiration.
- Examples: Covidien Shiley™ TaperGuard™, Teleflex™ SealGuard®.
- Advantage: Superior seal against micro-aspiration, potentially reducing the incidence of VAP. The tapered tip may also aid in smoother insertion.
4. Foam Cuffs
- Design: A cuff made of an open-cell foam material that is self-inflating. It has a pilot balloon and a one-way valve. When the 100% nitrogen in the foam is exposed to the air (which contains ~80% nitrogen), it re-expands.
- Mechanism: The foam expands to fill the anatomical contours of the trachea, creating a seal that conforms perfectly to the tracheal wall.
- Application: Almost exclusively used in tracheostomy tubes for long-term ventilation, not in standard ETTs. They provide an excellent seal but are impractical for short-term intubation.
Critical Clinical Note: Cuff Pressure Monitoring
Regardless of the cuff type, inflating the cuff by "feel" is dangerous and unreliable. Over-inflation can cause ischemia, while under-inflation can lead to leaks and aspiration.
The standard of care is to use a cuff pressure manometer to measure the pressure within the cuff after inflation. The target pressure is 20-30 cm H₂O. This simple, inexpensive device is essential for preventing cuff-related complications and ensuring patient safety during mechanical ventilation.
Back to 'Introduction to Endotracheal Tubes' →