The Pulmonary Artery Catheter (PAC), famously known by the brand name Swan-Ganz, is one of the most iconic—and now controversial—tools in the history of critical care medicine. It represents a monumental leap in our ability to directly measure intracardiac pressures and cardiac output.
Let's break it down completely.
Pulmonary Artery Catheter (Swan-Ganz)
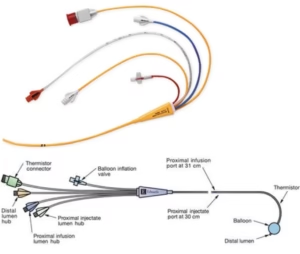 The Swan-Ganz catheter is a balloon-tipped, flow-directed catheter introduced through a central vein. Its primary purpose is to provide a comprehensive assessment of a patient's hemodynamic status by measuring pressures directly within the heart's chambers and the pulmonary artery.
The Swan-Ganz catheter is a balloon-tipped, flow-directed catheter introduced through a central vein. Its primary purpose is to provide a comprehensive assessment of a patient's hemodynamic status by measuring pressures directly within the heart's chambers and the pulmonary artery.
Principle of Operation
The genius of the Swan-Ganz design is its flow-directed nature. The catheter is advanced through a central vein (usually the internal jugular or subclavian) into the right atrium. A small balloon at the tip is then inflated with air (typically 1.5 cc). This balloon makes the catheter buoyant, allowing it to be "floated" by the flow of blood through the tricuspid valve, into the right ventricle, and then through the pulmonic valve into the pulmonary artery. The balloon is then deflated.
Components of a Swan-Ganz Catheter Kit
A standard PAC kit builds upon the basic CVC kit and includes several specialized components:
The Catheter Itself: A long (110 cm), multi-lumen catheter made of flexible plastic. It typically has 4-5 lumens (channels):
- Distal Port (Lumen): Opens at the very tip of the catheter. When the balloon is inflated and "wedged" in a branch of the pulmonary artery, this port measures the Pulmonary Artery Occlusion Pressure (PAOP), also known as Pulmonary Capillary Wedge Pressure (PCWP). When the balloon is deflated, it measures the Pulmonary Artery Pressure (PAP).
- Proximal Port (CVP Port): Opens about 30 cm back from the tip. When correctly positioned, this port sits in the right atrium and is used to measure the Central Venous Pressure (CVP) or Right Atrial Pressure (RAP). It's also used for fluid and medication administration.
- Balloon Inflation Port: A small lumen connected to a 1cc syringe used to inflate and deflate the distal balloon.
- Thermistor Connector/Lumen: This is the core of cardiac output measurement. It contains a fine-wire thermistor (temperature sensor) near the tip of the catheter. A known amount of cold saline is injected rapidly through the proximal port. The thermistor detects the change in blood temperature as it passes by. A computer (the cardiac output monitor) uses the temperature change over time (the thermodilution curve) to calculate the Cardiac Output (CO).
Introduction Sheath/Dilator: A larger sheath is often placed first to allow easy passage of the PAC and for rapid fluid/blood administration if needed.
Cardiac Output Monitor/Computer: A dedicated machine that connects to the thermistor wire and performs the thermodilution calculations.
Sterile Pressure Transducers: These devices convert the pressure from the fluid-filled catheters into an electrical signal that is displayed as a waveform on the monitor.
Uses and Key Hemodynamic Measurements
The PAC provides a wealth of data, both measured directly and calculated.
Direct Measurements:
- Central Venous Pressure (CVP): An estimate of right ventricular preload (volume status).
- Right Atrial Pressure (RAP): Often used interchangeably with CVP.
- Pulmonary Artery Pressure (PAP): Measures pressure in the pulmonary artery. Gives both a systolic and diastolic value.
- Pulmonary Artery Occlusion Pressure (PAOP / PCWP): This is the most crucial measurement. When the balloon is wedged, it stops flow beyond it, creating a static column of blood between the catheter tip and the left atrium. Therefore, the PAOP is an excellent surrogate for Left Atrial Pressure (LAP), which itself is a surrogate for Left Ventricular End-Diastolic Pressure (LVEDP)—the true measure of left ventricular preload.
Calculated Parameters (using the above values and patient data):
- Cardiac Output (CO): The volume of blood pumped by the heart per minute (L/min).
- Cardiac Index (CI): Cardiac Output adjusted for body surface area (L/min/m²), allowing for comparison between patients of different sizes.
- Stroke Volume (SV): The amount of blood pumped with each beat (CO / Heart Rate).
- Systemic Vascular Resistance (SVR): The resistance the left ventricle has to pump against to get blood to the body. An indicator of afterload.
- Pulmonary Vascular Resistance (PVR): The resistance the right ventricle has to pump against to get blood to the lungs.
Clinical Indications (Historically):
- Differentiating cardiogenic vs. non-cardiogenic shock (e.g., ARDS).
- Guiding therapy in severe heart failure (especially right heart failure).
- Managing complex cases of septic shock.
- Assessing and managing severe pulmonary hypertension.
- Monitoring high-risk cardiac surgery patients.
Why the Swan-Ganz Catheter Has Become Redundant
Once considered the pinnacle of hemodynamic monitoring, the routine use of the PAC has plummeted. It is now considered a niche tool, used only in very specific circumstances by experts. This decline is due to several converging factors:
1. Lack of Proven Mortality Benefit: This is the single biggest reason. Multiple large, randomized controlled trials (e.g., the ESCAPE trial for heart failure) failed to demonstrate that using a PAC to guide therapy improved patient survival or outcomes compared to clinical assessment alone. In some cases, it was associated with worse outcomes, likely due to complications and misinterpretation of data.
2. High Risk of Complications: The PAC is more invasive and carries more risks than a standard CVC.
- Arrhythmias: The catheter can irritate the heart's conduction system, causing ventricular tachycardia or fibrillation.
- Rupture of a Pulmonary Artery: A catastrophic and often fatal complication if the balloon is over-inflated or advanced too far.
- Pulmonary Infarction: If the catheter remains wedged for too long.
- Infection and Thrombosis: Similar to other central lines, but the longer dwell time and complexity increase the risk.
3. Interpretation is Difficult and Prone to Error: The data from a PAC is not straightforward. PAOP can be falsely elevated by mitral valve disease or high positive-pressure ventilation. CVP is a notoriously poor indicator of volume status. Misinterpreting these numbers can lead to harmful therapeutic decisions, such as giving fluids to a patient in pulmonary edema or withholding them from a patient who is truly hypovolemic.
4. The Rise of Less Invasive, More Dynamic Technologies: Modern medicine has developed superior alternatives that are safer and often provide more useful information.
- Transthoracic & Transesophageal Echocardiography (TTE/TEE): Ultrasound provides a direct, real-time view of cardiac function, valve status, chamber size, and can estimate filling pressures and cardiac output. It is dynamic, repeatable, and non-invasive (TTE) or minimally invasive (TEE).
- Minimally Invasive Cardiac Output Monitors (e.g., PiCCO, LiDCO): These systems use arterial waveform analysis and often require a central line and a special arterial catheter, but not a PAC. They provide continuous data on cardiac output, stroke volume variation (a dynamic measure of fluid responsiveness), and extravascular lung water.
- Bioreactance/Impedance Cardiography: Completely non-invasive sensors placed on the chest to estimate cardiac output.
5. A Paradigm Shift in Hemodynamic Understanding: Critical care has moved away from relying on static pressure values (like CVP and PAOP) to guide fluid therapy. The focus is now on fluid responsiveness—determining if a patient's heart will actually increase its stroke volume if given a fluid bolus. This is better assessed with dynamic tests like a Passive Leg Raise (PLR) or measuring Stroke Volume Variation (SVV) on a ventilated patient, which are provided by modern monitors.
Current Role
The Swan-Ganz is not entirely extinct. It is still used in very specific, expert-level scenarios where precise measurements of pulmonary artery pressures and cardiac output are essential and cannot be obtained by other means, such as:
- Management of severe pulmonary hypertension (e.g., initiating IV therapy).
- Evaluation for heart transplantation or LVAD implantation.
- Complex congenital heart disease.
- Rare cases of shock where the diagnosis remains unclear after all other modalities.
In summary, the Swan-Ganz catheter was a revolutionary tool that taught us an immense amount about cardiovascular physiology. However, its routine use has been abandoned due to a lack of outcome benefit, significant risks, and the emergence of safer, less invasive, and more physiologically relevant technologies.