The Lifeline in the Neck: Understanding the Tracheostomy Tube & Set
In the hierarchy of medical interventions, few are as immediate and life-sustaining as securing an airway. While endotracheal intubation is common for short-term needs, the tracheostomy provides a stable, long-term solution. At the heart of this procedure is the tracheostomy tube & set—a collection of precision-engineered components that serves as a direct portal to the trachea, enabling breathing, ventilation, and life itself.
This post delves into the anatomy, types, and purpose of this essential medical device.
Why a Tracheostomy? The Core Indications
A tracheostomy is a surgically created opening (stoma) through the neck into the trachea (windpipe). A tracheostomy tube is inserted to keep this airway patent. The primary reasons for performing this procedure include:
- Prolonged Mechanical Ventilation: The most common indication in the ICU. For patients expected to need a ventilator for more than 7-14 days, a tracheostomy is more comfortable, secure, and allows for better weaning from the ventilator compared to an endotracheal tube.
- Upper Airway Obstruction: A blockage above the level of the trachea (e.g., from a tumor, severe trauma, infection, or angioedema) that prevents air from reaching the lungs.
- Airway Protection: For patients who cannot protect their own airway from aspiration (e.g., due to neurological injury or stroke), a cuffed tracheostomy tube can seal the airway and prevent secretions or food from entering the lungs.
- Facilitation of Airway Clearance: Patients with neuromuscular diseases (like ALS or spinal cord injury) or those with excessive secretions may require a tracheostomy to enable effective suctioning of the trachea.
Anatomy of a Tracheostomy Tube
A standard tracheostomy tube is a sophisticated device with several key components, each serving a specific function.
1. Outer Cannula: This is the main body of the tube that stays in the trachea. It has three key parts:
- Shaft: The portion that sits inside the trachea. It is curved to match the anatomy of the neck.
- Flange (or Neck Plate): The flat plate that rests against the neck. It has holes to secure the tube with tracheostomy ties or a holder, preventing it from being dislodged or falling into the airway.
- Cuff (Inflatable Balloon): Located near the distal tip of the outer cannula. When inflated with air via the pilot line, it creates a seal against the tracheal wall. This seal is critical for delivering positive-pressure ventilation and preventing aspiration. Modern cuffs are high-volume, low-pressure cuffs, which distribute pressure over a larger area to minimize the risk of tracheal wall injury.
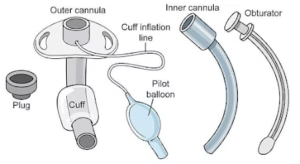
2. Inner Cannula: This is a smaller, removable tube that fits snugly inside the outer cannula.
- Purpose: Its primary function is to collect secretions and can be easily removed for cleaning without having to change the entire outer tube. This significantly reduces the risk of tube obstruction from mucus plugging.
- Types: They can be reusable (cleaned regularly) or disposable (replaced as needed).
3. Pilot Balloon & Inflation Line: A small, external balloon connected to the main cuff by a thin tube. The amount of air in the pilot balloon corresponds to the amount of air in the cuff, allowing clinicians to monitor cuff inflation without a manometer.
4. Obturator: A tapered, solid plastic or silicone tool that fits inside the outer cannula during insertion. Its smooth, rounded tip guides the tube into the trachea without damaging the delicate tissues. It is removed immediately after the tube is in place.
5. 15mm Connector: The standard connector at the proximal end of the tube, which allows it to attach to a ventilator circuit, bag-valve mask, or speaking valve.
The "Set": More Than Just a Tube
A tracheostomy procedure requires more than just the tube itself. A complete tracheostomy set includes all the instruments needed for the surgical procedure and initial care:
- Scalpel & Blade
- Tracheal Hook (to lift the trachea)
- Tracheal Dilator (to widen the stoma)
- Forceps and Retractors
- Suction Catheter (to clear secretions)
- Tracheostomy Tube Holder or Ties
Types of Tracheostomy Tubes
The versatility of the tracheostomy tube lies in its many variations, designed to meet specific patient needs.
Type | Description | Primary Use |
|---|---|---|
| Cuffed vs. Uncuffed | Cuffed: Has an inflatable balloon. Uncuffed: No balloon. | Cuffed: For ventilation or airway protection. Uncuffed: For patients who can breathe independently and protect their airway (e.g., weaning, long-term sleep apnea). |
| Fenestrated | Has one or more holes ("fenestrations") on the outer curve of the outer cannula. | To allow airflow through the upper airway, enabling the patient to speak and cough more effectively when the cuff is deflated and the inner cannula is removed. |
| Single Cannula | Does not have a removable inner cannula. | Often used in pediatric sizes or for patients with very narrow airways where a smaller inner diameter is critical. |
| Adjustable Flange | The flange can be moved along the shaft of the tube. | For patients with difficult anatomy, such as those with a very thick neck (obesity) or a deep-seated trachea. |
| Metal Tubes | Made of silver or stainless steel. | For long-term or permanent use in patients who are well-established with their tracheostomy. They are durable but lack a cuff. |
Care and Potential Complications
A tracheostomy is a life-saving but invasive procedure that requires meticulous care to prevent complications.
- Care Includes: Regular stoma cleaning, humidification of inspired air (the nose and upper airway normally do this), monitoring cuff pressure, and frequent suctioning.
- Complications Can Be:
- Early: Bleeding, tube obstruction, infection, and accidental decannulation (tube falling out).
- Late: Tracheal stenosis (narrowing of the windpipe), formation of granulation tissue, and in rare cases, a tracheo-innominate artery fistula (a life-threatening hemorrhage).
Conclusion
The tracheostomy tube and set represent a pinnacle of airway management technology. It is a device that transitions a patient from the acute, high-dependency environment of the ICU to a state of stability, whether in the hospital, a rehabilitation facility, or even at home. Understanding its components, types, and purpose is fundamental for anyone involved in the care of these patients, as this simple-looking tube is, quite literally, the lifeline in their neck.