Anesthesia Machine & Anesthesia Workstation
 Welcome to the nerve center of the operating room. The anesthesia workstation, with its complex array of dials, circuits, and monitors, can seem like an intimidating beast. But what if you could master it? This comprehensive resource is your guide on a fascinating journey—from the historic, clunky elegance of the Boyle's machine to the sleek, intelligent workstations of Dräger, GE, and Mindray that define modern practice. We will demystify the physics, deconstruct the components, and build your confidence. This isn't just about learning a machine; it's about understanding your most critical partner in ensuring patient safety.
Welcome to the nerve center of the operating room. The anesthesia workstation, with its complex array of dials, circuits, and monitors, can seem like an intimidating beast. But what if you could master it? This comprehensive resource is your guide on a fascinating journey—from the historic, clunky elegance of the Boyle's machine to the sleek, intelligent workstations of Dräger, GE, and Mindray that define modern practice. We will demystify the physics, deconstruct the components, and build your confidence. This isn't just about learning a machine; it's about understanding your most critical partner in ensuring patient safety.
Our journey will be a methodical one. We'll start by laying a strong foundation, exploring the history and the core physics that govern every machine. From there, we'll build up your knowledge piece by piece, dissecting the classic anatomy of an anesthesia machine and mastering the circle breathing system. Only then will we leap into the modern era, comparing the sophisticated features of today's leading workstations. Each module is designed to build upon the last, transforming a daunting subject into a clear, manageable, and ultimately, masterable skill.
Advanced Techniques in Anesthesia
Modern anesthesia has evolved into a high-tech discipline of precision, far surpassing the sedation of the past. By utilizing ultrasound for targeted nerve blocks, computerized pumps for intravenous drug delivery, and brain monitors to gauge consciousness, anesthesiologists can now tailor care to individual physiology. Advanced airway devices and rapid-reversal agents further enhance safety and recovery, redefining the anesthesiologist’s role from a passive observer to an active architect of the patient’s surgical journey.
Temperature Probe (Nasopharyngeal, Esophageal)
Nasopharyngeal and esophageal temperature probes are medical devices used to measure a patient’s core body temperature. Unlike a standard oral or forehead thermometer, these probes provide a highly accurate and continuous measurement of the temperature of the body’s vital organs.
The 19th-Century Anesthesia

Before the mid-19th century, surgery was a brutal spectacle of speed and screaming. The introduction of ether and chloroform changed everything, replacing agony with relief. By allowing surgeons to operate with precision rather than haste, anesthesia transformed medicine from a butcher’s trade into a sophisticated, life-saving discipline.
Local Anesthetic Agents

Local anesthetics provide reversible anesthesia by blocking voltage-gated sodium channels, halting nerve conduction. Their clinical profile—onset, potency, and duration—is determined by chemical structure, distinguishing amides from esters. While indispensable for surgery and pain management, their narrow therapeutic index mandates vigilant dosing and monitoring to prevent life-threatening systemic toxicity.
Ropivacaine
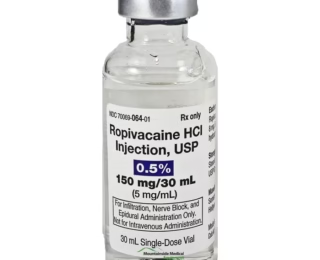
Ropivacaine is a long-acting amide local anesthetic known for its improved safety profile compared to bupivacaine. It provides potent sensory anesthesia with relative motor-sparing effects and has significantly lower cardiotoxicity. It is a primary choice for peripheral nerve blocks and labor epidurals.
Lidocaine (Lignocaine)
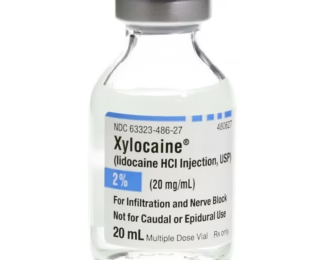
Lidocaine is a versatile amide local anesthetic and Class Ib antiarrhythmic. It provides local and regional anesthesia, treats ventricular arrhythmias, and is used intravenously for analgesia and to blunt sympathetic responses. Its narrow therapeutic index mandates careful dosing and vigilant monitoring for signs of toxicity.
Glycopyrrolate
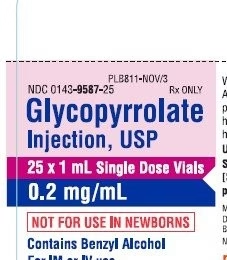
Glycopyrrolate is a quaternary anticholinergic used to reduce secretions, treat bradycardia, and prevent side effects of neuromuscular reversal. It reliably causes tachycardia by blocking vagal tone and, because it does not cross the blood-brain barrier, it lacks central nervous system effects, making it ideal for perioperative use.
Neostigmine

The standard reversal agent for non-depolarizing neuromuscular blockade, Neostigmine inhibits acetylcholinesterase. It requires mandatory co-administration with an anticholinergic to prevent bradycardia and secretions. Objective confirmation of adequate reversal with a nerve stimulator is essential before considering extubation.
Disclaimer!
The information provided on this platform, including but not limited to articles, case studies, clinical scenarios, guidelines, and multimedia content, is intended for educational and informational purposes only.
The authors and editors of this material have made every effort to ensure the accuracy of treatments, drugs, and dosage regimens that conform to currently accepted standards. However, due to continual changes in information resulting from ongoing research and clinical experience, unique aspects of individual clinical situations, as well as the potential for human error; readers must exercise personal judgment when making a clinical decision.
This website may contain third-party information or links to other internet websites. We do not control nor assume responsibility for any third-party content provided nor content on linked Internet websites.
We strongly recommend the visitors of this website to go through its Detailed 'Disclaimer' and 'Terms of Use'.
By accessing, browsing, or using this website, you acknowledge that you have read, understood, and agreed to be bound by the 'Disclaimer' and 'Terms of Use'. If you do not agree with these terms, you must NOT use this website.